When couples start fertility treatment, one of the first questions that arises is what is the difference between icsi and ivf. Both are assisted reproductive technologies designed to help achieve pregnancy, but they differ mainly in how fertilization occurs.
Understanding these differences helps patients make confident, informed choices about which procedure fits their situation.
IVF: The Classic Approach
In conventional IVF, mature eggs are retrieved and placed in a laboratory dish with thousands of sperm. The strongest sperm naturally fertilize the egg.
This process mimics natural conception, just outside the body. IVF is often used for unexplained infertility, blocked tubes, or cases where sperm count and motility are normal.
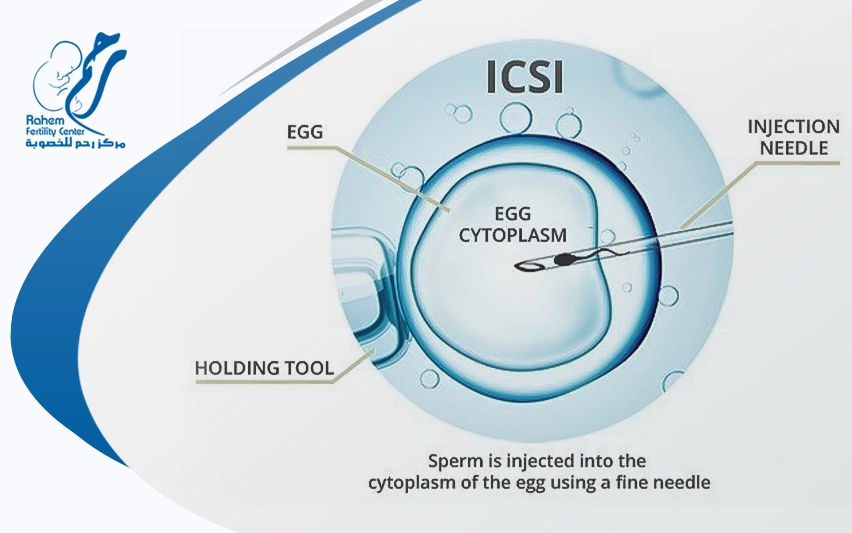
ICSI: Precision Fertilization
ICSI, short for Intracytoplasmic Sperm Injection, is a more targeted method. Instead of leaving fertilization to chance, an embryologist injects a single healthy sperm directly into an egg using a microneedle.
This technique was developed to overcome severe male factor infertility, such as low sperm count or poor motility.
For couples struggling with sperm-related issues, ICSI can make a major difference in success rates.
What is the difference between ICSI and IVF in practice?
The main difference lies in control and indication. IVF relies on sperm competition, while ICSI bypasses it entirely.
Both methods use the same overall structure: ovarian stimulation, egg retrieval, fertilization, embryo culture, and transfer, but ICSI adds a crucial lab step. The goal of both is the same: creating viable embryos for transfer and pregnancy.
For a step-by-step overview of what happens before fertilization, you can explore the IVF Timeline to see how each stage fits into the full process.
Which is more expensive, ICSI or IVF?
Cost is another key concern when comparing treatments. Many patients ask, Which is more expensive, ICSI or IVF? Since ICSI requires additional lab expertise and specialized micromanipulation equipment, it typically costs more.
The price difference varies by clinic and country, but ICSI can add several hundred to over a thousand dollars per cycle.
However, the higher cost can be justified if male infertility is a factor or if previous IVF cycles have failed to achieve fertilization.
When evaluating expenses, patients also consider medication costs, such as those discussed in IVF injection price, since they can significantly affect the total budget.
When is ICSI recommended?
Clinics usually recommend ICSI for:
- Severe male factor infertility (low count, motility, or morphology).
- Previous IVF cycles with poor fertilization.
- Frozen or surgically retrieved sperm.
- Limited egg numbers (e.g., diminished ovarian reserve).
Still, some clinics apply ICSI more broadly to reduce the chance of total fertilization failure. The decision should always balance medical need and financial impact.
ICSI vs. IVF: Choosing the Right Fertility Path for Your Journey
Understanding what is the difference between icsi and ivf isn’t just about lab technique; it’s also about treatment goals, success rates, and personal circumstances.
Both procedures share the same foundation, but the decision to add ICSI depends on medical history and prior results.
Get your inquiry
At Rahem Center, our vision is to be at the forefront of distinguished scientific centers in the field of fertility assistance, not only in Egypt but in the world.
Can you have IVF without ICSI?
Yes. Traditional IVF works well when sperm quality is normal and fertilization occurs naturally in the lab. ICSI is used only when needed, mainly for male factor infertility or past fertilization issues. It’s a precise option, not a default step.
Can you do mini IVF with ICSI?
Yes. Mini IVF uses lower stimulation to produce fewer, high-quality eggs, which can be fertilized through ICSI if sperm quality is low.
This combination helps maximize results per egg and is often chosen for patients with low ovarian reserve or mild male infertility.
Which option offers better success?
When evaluating what is the difference between icsi and ivf, success rates depend less on the technique itself and more on the underlying cause of infertility.
- If sperm parameters are normal, success rates between IVF and ICSI are often similar.
- If sperm quality is compromised, ICSI may significantly improve outcomes by ensuring fertilization occurs.
- Both methods depend on egg quality, embryo development, and uterine health rather than the lab step alone.
Balancing science, cost, and personal fit
The ultimate goal of both procedures is the same: a healthy embryo and a successful pregnancy. While ICSI adds precision, it also increases costs, and not every case benefits from it.
Patients should discuss with their fertility team whether ICSI offers a medical advantage or is simply elective.
Understanding what is the difference between icsi and ivf helps couples make decisions grounded in data rather than fear, balancing medical advice with financial readiness.
Rahem Fertility Center: Guiding You Toward the Right Fertility Choice
At Rahem Fertility Center, we help couples understand every detail from how fertilization happens to deciding between IVF and ICSI. Our experts combine advanced technology with compassionate care to design treatment plans tailored to your needs.
If you’re ready to take the next step, book your consultation today and let us guide your journey toward parenthood with confidence and clarity.